Multidirectional Instability
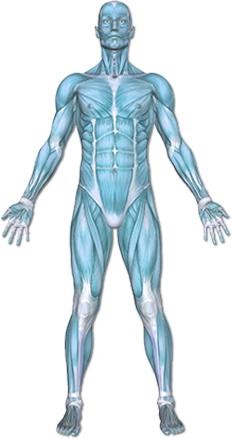
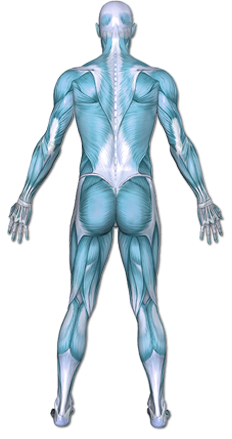
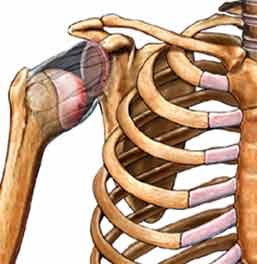
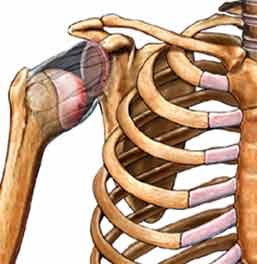
Shoulder instability occurs when the upper-end of the arm bone, known as the humerus, slides partially or completely out of the shoulder socket.
The disorder is classified by how much the humerus moves and the direction of the movement:
• Subluxation—The humeral head moves part way out of the shoulder socket.
• Dislocation—The humeral head moves completely out of the socket.
• Anterior—The humeral head moves toward the front.
• Posterior—The humeral head moves toward the back.
• Multidirectional
Copyright © Nucleus Medical Media, Inc.
This content was created using EBSCO’s Health Library
Shoulder instability often results from injury. Multi-directional instability may be from repetitive injury or from congenital ligamentous laxity.
This content was created using EBSCO’s Health Library
Factors that increase the risk of shoulder instability include:
- Previous shoulder dislocation
- Athletic activity, especially:
- Baseball—pitching
- Football—tackling
- Tennis
- Gymnastics
- Weight-lifting
- Any collision or contact sport
- Volleyball
- Swimming, especially backstroke or butterfly
- Congenital collagen disorders, such as:
- Marfan syndrome—a connective tissue condition
- Ehlers-Danlos syndrome—a condition in which patients have loose joints
- Hereditary Conditions
This content was created using EBSCO’s Health Library
Symptoms may come on suddenly or develop over time. Symptoms may include:
- Pain in the shoulder area
- Shoulder or arm weakness
- Shoulder may feel loose
- Shoulder may slip out of place
- Numb feeling down the arm
This content was created using EBSCO’s Health Library
You will be asked about your symptoms and medical history. A physical exam will be done. Special attention will be given to your shoulders. Your doctor will determine your range of motion and try to move the humeral head within the socket. Your shoulder may need to be viewed internally. This can be done with:
- X-rays
- MRI scan
- CT scan
- Arthroscopy
This content was created using EBSCO’s Health Library
- Non-surgical treatment will focus on reducing the strain at the shoulder in a downward or backward position during functional task performance. The therapist will likely present a number of restricted motions and ways to perform functional daily tasks without putting strain on the ligaments. In the case of a painful shoulder, the therapist will recommend anti-inflammatory techniques and positions of the shoulder at night and during sustained or repetitive task performance. The therapist will recommend strengthening exercises to the support muscles in order to improve safe reach and reduce the risk of recurrent dislocation.
- Following a surgical procedure, the therapist will work closely with the surgeon to determine the safe motion patterns and range of motion. If the arm is kept still too long, the tightening procedure that was performed could limit the motion too much. If the shoulder is allowed to move too quickly, the ligaments could stretch back out and continue to cause the MDI.
This content was created using EBSCO’s Health Library
Guidelines to help protect the shoulder from injury include:
- Doing regular exercises to strengthen the supporting muscles
- Using proper athletic training methods
- Increasing the duration or intensity of your exercises gradually
- Modifying activities to prevent excessive external rotation and overhead motions of the shoulder
This content was created using EBSCO’s Health Library
This content was created using EBSCO’s Health Library
RESOURCES:
- American Academy of Family Physicians
- American Academy of Orthopaedic Surgeons
CANADIAN RESOURCES:
- Canadian Orthopaedic Association
- Canadian Orthopaedic Foundation
REFERENCES:
- Abrams GD, Safran MR. Diagnosis and management of superior labrum anterior posterior lesions in overhead athletes. Br J Sports Med. 2010 Apr;44(5):311-318.
- Dumont GD, Russell RD, et al. Anterior shoulder instability: a review of pathoanatomy, diagnosis, and treatment. Curr Rev Musculoskelet Med. 2011 Aug 2.
- Gaskill TR, Taylor DC, et al. J Am Acad Orthop Surg. 2011 Dec 19(12):758-767.
- Luime JJ, Verhagen AP, et al. Does this patient have an instability of the shoulder or a labrum lesion? JAMA. 2004;292:1989-1999.
- Mahaffey BL. Smith PA. Shoulder instability in young athletes. Am Fam Physician. 1999;59:2773.
- Provencher MT, Frank RM, et al. The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg. 2012 Apr;20(4):242-252.
- Recurrent subluxation of shoulder. EBSCO DynaMed website. Available at: https://dynamed.ebscohost.com. Updated September 6, 2012. Accessed November 21, 2013.
- van Tongel A, Karelse A, et al. Posterior shoulder instability: current concepts review. Knee Surg Sports Traumatol Arthrosc. 2011 Sep;19(9):1547-1553.
- von der Heyde RL. Occupational therapy interventions for shoulder conditions: a systematic review. Am J Occup Ther. 2011 Jan-Feb;65(1):16-23.
- Wolf JM, Cameron KL, et al. Impact of joint laxity and hypermobility on the musculoskeletal system. J Am Acad Orthop Surg. 2011 Aug;19(8):463-471.
This content was created using EBSCO’s Health Library