Low Back Pain
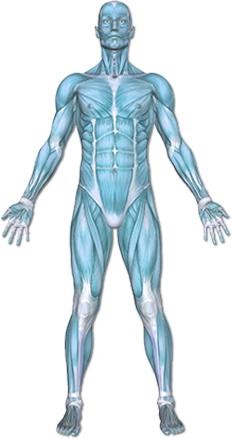
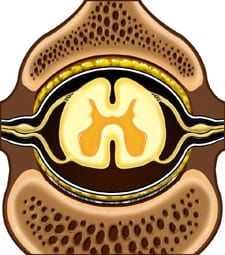
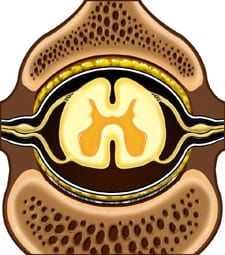
Low back pain is an ache or discomfort in the lower part of the spinal column. It may radiate down into one or both legs. The lower spinal column consists of small, stacked bones (vertebrae) that surround and protect the spinal cord and nerves.
Copyright © Nucleus Medical Media, Inc.
This content was created using EBSCO’s Health Library
There are many possible causes for low back pain, including:
- Sprain or strain of muscles or ligaments in the area
- Herniated disc or ruptured disc—the cushions between the bones of the spine bulge out of place as a result of age-related changes or trauma.
- Disc degeneration—caused by arthritis or aging
- Lumbar spinal stenosis —bony narrowing of the spinal canal in the low back area
- Spondylolysis —fracture of part of the a bone in the back
- Spondylolisthesis —slippage of one bone over another, causing stretching or pinching of nerves
- Fractures due to trauma or osteoporosis
- Fibromyalgia —a condition that causes muscle aches and fatigue
- Ankylosing spondylitis —a disorder that causes spine stiffness and arthritis (believed to be hereditary)
- In rare cases,
- Benign or malignant tumors
- Infections
- Arterial problems, such as hardening of the arteries
This content was created using EBSCO’s Health Library
A risk factor is something that increases your likelihood of getting a disease or condition. It is possible to develop low back pain or sciatica with or without the risk factors listed below. However, the more risk factors you have, the greater your likelihood of developing low back pain or sciatica. If you have a number of risk factors, ask your doctor what you can do to reduce your risk. Risk factors include: Overuse of the back muscles during any activity.
Scoliosis
Scoliosis is an abnormal curvature of the spine that can cause low back pain, especially in adults.
Sedentary Job or Lifestyle
Muscles that support the back can become weak with lack of exercise.
Occupation
Work that requires the following motions puts additional stress on the back:
- Heavy lifting
- Bending or twisting
- Exposure to vibrations, such as riding in a car or operating heavy machinery
Participating in Strenuous or Contact Sports
- Injuries from contact sports or falls can result in back pain.
- High-impact sports, for example, distance running
Cigarette Smoking
Smoking may cause discs in the spine to wear down.
Obesity
Maintaining a healthy weight is important for your overall health. Extra weight can increase pressure on the spinal muscles and disks.
Improper Lifting Techniques
When you lift objects with your back muscles instead of the stronger muscles in your legs, you increase your risk of back injury.
Age
As you grow older, the disks in your back begin to lose water content and degenerate. This increases the risk of disk problems and back pain, especially after age 40. However, even with some disk degeneration, most people do not have back pain.
Psychosocial factors
Stress, anxiety, and negative mood may increase your risk of low back pain
This content was created using EBSCO’s Health Library
The pain can be achy or sharp in nature. It is usually localized in the low back and can be associated with difficulty doing everyday tasks. Stress on the muscles and ligaments that support the spine produce strain on tissues causing back pain. There can also be other, more serious causes. If a nerve is irritated, the pain may extend into the buttock or leg on the affected side, and weakness or numbness may be present. Other symptoms may include burning, tingling, or a shooting pain down the back of one leg. This is often called “sciatica.” However, the nerve involved is usually a spinal nerve, and only occasionally the sciatic nerve. Sciatica is known by many other medical terms, such as lumbosacral radicular pain or radiculopathy. More serious symptoms associated with back pain that may require immediate medical attention include:
- Pain that doesn’t subside or worsens with rest
- Pain that is worse when you are reclined
- Pain that is sudden, severe, or that has gotten dramatically worse
- Progressive weakness or numbness in a leg or foot
- Difficulty walking, standing, or moving
- Numbness in the genital or rectal area
- Loss of bowel or bladder control
- Burning or difficulty with urination
- Fever, unexplained weight loss, or other signs of illness
- If there has been any trauma, fall, or impact
- If you have a history of cancer, back pain should be evaluated
This content was created using EBSCO’s Health Library
Your healthcare provider will ask about your symptoms and medical history. A physical exam will be done. Your back, hips, and legs and will be tested for strength, flexibility, sensation, and reflexes. Often, patients with pain may feel an urgent need to have a medical test. Medical tests are not routinely required for back pain and sciatica. With therapy, most episodes of acute back pain resolve over several weeks. In these cases, the information from an x-ray or MRI scan may not change the medical plan, so tests may be unnecessary. An MRI scan or x-ray is usually ordered if there is a plan to do a procedure or surgery based on the result of the images. Studies of medical imaging have demonstrated that MRI scan and x-ray may be too sensitive. They can often show abnormalities that are not truly significant, such as degenerated discs in individuals who do not have symptoms. An improper medical test can lead to improper treatment and can greatly increase medical costs. It is important for such tests to be ordered appropriately. Tests may include:
- X-ray—Back x-rays may show signs of arthritis, degenerative disk disease, osteoporosis, infections (such as tuberculosis), fractures, dislocations, or evidence of a tumor.
- CT scan—CT scans may show disc herniations as well as tumors and other lesions. It is more sensitive than x-ray.
- MRI scan—An MRI scan can show if a disc has herniated, and if there are signs of scar tissue around a nerve root. The test can detect other abnormalities, such as bony spurs pressing on a nerve root and tumors. It is more sensitive than a CT scan.
- Blood tests—Blood tests may include a complete blood count and sedimentation rate. Blood tests may be ordered to check for signs of infection, metabolic disease, or inflammation.
- Urine test—These tests check for urinary infection or blood in the urine.
- Nerve conduction study—To determine the health or disease of a nerve.
- Electromyography—To determine if the nerve going to a muscle is functioning normally or if there may be pressure on it. It is often performed in conjunction with a nerve conduction study.
- Myelography—X-rays are then taken to see how the dye lines the space in the spinal canal and if there are disc herniations or other lesions. This test may be ordered before performing back surgery.
- Biopsy—If imaging studies determine that the cause of your back pain appears to be the result of a tumor, your physician may take a piece of the tumor (a biopsy). This will help determine what kind it is and how best to treat it.
This content was created using EBSCO’s Health Library
Your therapist will educate you on pain-relieving techniques (such as ice) and decreasing or modifying painful activities. This diagnosis often occurs from muscular tightness or weakness which causes posture to get out of alignment. Your therapist will educate and assist in proper stretching and strengthening exercises for the back. They may need to perform hands on, manual therapy techniques to further increase joint flexibility. The final phase of rehab will involve strengthening during functional activities and education to prevent the injury from occurring again.
This content was created using EBSCO’s Health Library
You can reduce your risk of developing low back pain and sciatica by reducing the stress on your back. Guidelines for reducing stress on your back include:
- Support your back when lifting, standing, and sitting.
- Practice good posture.
- Lose weight if you are overweight.
- Exercise regularly.
- If you smoke, quit.
- Manage stress.
Support Your Back When Lifting, Standing, and Sitting Guidelines include:
- Do not lift heavy objects alone.
- Plan ahead and ask for assistance with lifting or moving heavy objects.
- When lifting, squat down next to the object, hold the object close to your chest, maintain a straight back, and use your leg muscles to slowly rise.
- Avoid excessive, prolonged, or forceful bending or twisting of your back.
- Avoid sitting for long periods. When you do sit, choose seats with good lumbar support, and use a footstool to raise your knees to hip level. You may be able to use a standing desk at intervals, to help avoid prolonged sitting.
- Avoid standing for long periods. If you need to stand, place a low footstool in front of you and alternate placing each foot on it for a period of time. This will take some of the load off your back.
- Do not drive for long periods. Take a break every hour to stop, get out of the car, and stretch your back.
Practice Good Posture
Poor posture and slouching can put pressure on your lower back. Stand and sit straight, and avoid sitting up in bed. If possible, find an ergonomic specialist to help teach you good posture and body mechanics, as well as help you redesign your workplace to reduce strain on your back.
Lose Weight If You Are Overweight
Maintenance of good weight is important for your overall health. While scientific evidence is inconclusive as to how much obesity contributes to back pain in general, extra pounds can increase pressure on the spinal muscles and disks. Follow the dietary and exercise plan recommended by your doctor. To lose weight you have to consume fewer calories than you expend. To maintain a healthy weight, eat an equal number of calories to those you expend. Even more exercise than minimum recommendations may be required to lose weight (see below).
Exercise Regularly
An aerobic program will improve your physical fitness, strengthen your back muscles, and help you maintain a healthy weight. Choose exercises or activities that you enjoy and will make a regular part of your day. For most people, this could include walking or participating in another aerobic activity for 30 minutes per day. The 2008 USDA Physical Activity Guidelines Advisory Committee Report recommends at minimum two hours and 30 minutes a week of moderate aerobic activity, and strengthening exercises at least two days a week. Exercise also can help you manage stress. Check with your doctor before starting any exercise program.
If You Smoke, Quit
Smoking may contribute to degeneration of the discs in the spine. Also, smokers risk possible re-injury to the back during a coughing attack. Smoking can adversely affect healing if you are having a back surgery. To heal properly, you should quit smoking two weeks before a spine fusion and stay tobacco-free for six months afterwards.
Manage Stress
Stress can increase muscle tension. Take time out to relax, exercise, and practice relaxation techniques. If you need support or assistance in reducing stress, you may want to try some of the following techniques:
- Cognitive behavioral therapy
- Counseling
- Stress management classes
- Relaxation techniques
- Breathing exercises
- Meditation
- Yoga
This content was created using EBSCO’s Health Library
This content was created using EBSCO’s Health Library